Which SUD Treatments are Truly 'Evidence-Based' Practices?
The term “Evidence-Based” is all the rage these days. We use the term ourselves, although we strive not to use it loosely. In that spirit we have augmented our website to offer greater transparency and specifics on the evidence that supports R1 Learning content. Additionally, we are regularly diving more deeply into the concept of Evidence-Based Practices and publishing articles on our website. In the first three posts of this ‘Evidence-Based’ blog series we looked at the following:
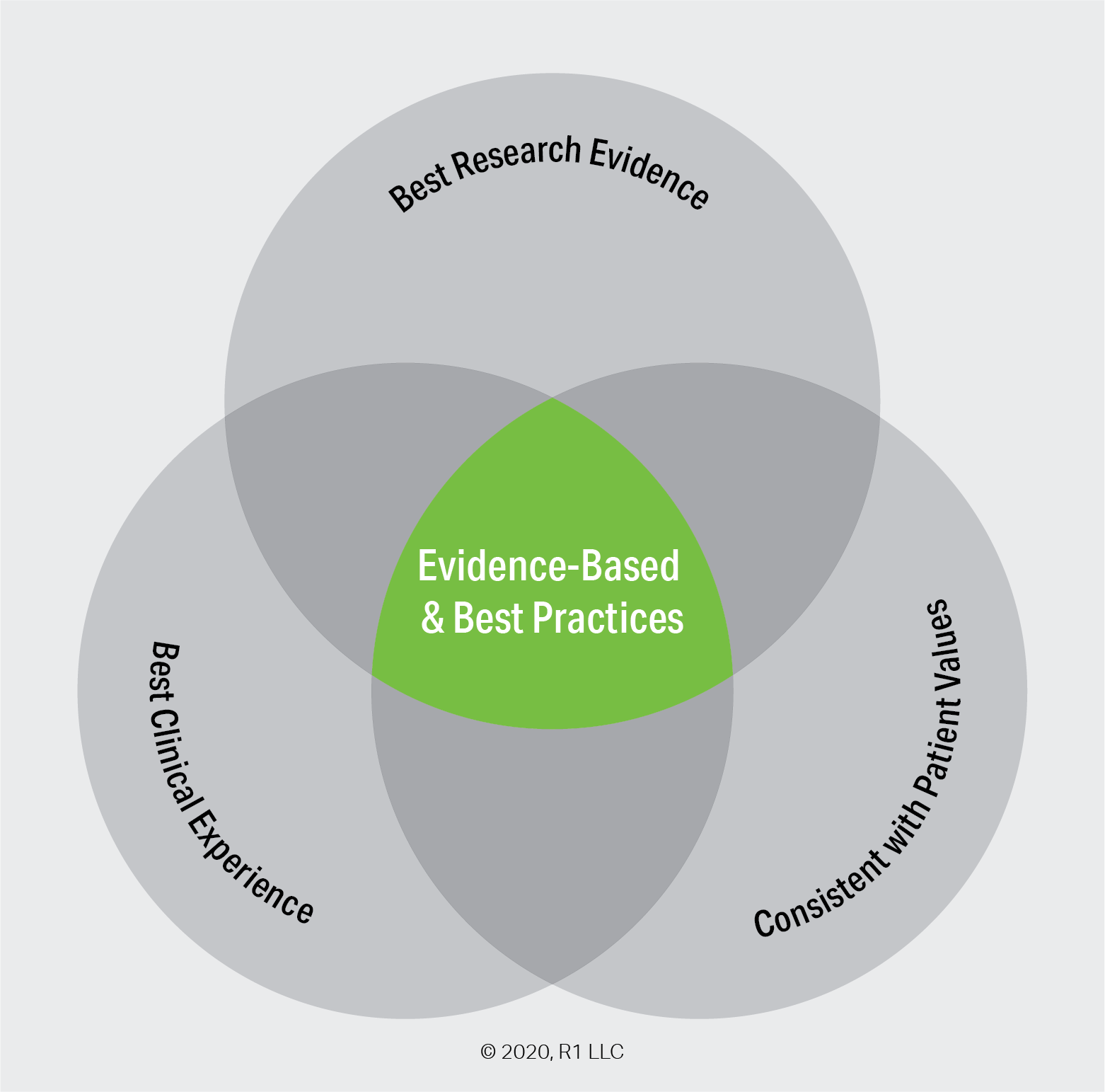
What Does ‘Evidence-Based’ Practice Really Mean? We see and hear the term all the time. What exactly does it mean?.
Upon What Evidence Are Evidence-Based Practices Based? There are many forms of ‘evidence’ and a hierarchy for ranking the different types.
What Did That Big Alcoholics Anonymous Study Really Study? Mainstream media outlets covered the release of a major study on the effectiveness of Alcoholics Anonymous. What type of evidence was this study and were the headlines an accurate interpretation of the study?
In addition to delving into the details of a systematic review, the AA study also presented an opportunity to look at one of the ‘consensus’ evidence-based practices for substance use disorder, namely Twelve-Step Facilitation (TSF) therapy. Today we want to briefly discuss seven other ‘consensus’ evidence-based behavioral therapies.
Why the emphasis on ‘Evidence-Based’ treatment?
There are a number of key reasons for the widespread emphasis on the use of evidence-based practices for substance use disorder. The first is the most important in our minds.
More effective: As the U.S. Surgeon General bluntly stated, “Treatments using these evidence-based practices have shown better results than non-evidence-based treatments and services.”
Grant Awards: SAMHSA and other grantmaking bodies strongly favor - if not outright require - that grants be used for evidence-based treatment strategies.
Insurance Reimbursement: Decades of legislation at both the national and state level have been pushing insurance companies toward “Mental Health Parity”, meaning coverage and reimbursement of mental health must be equal to those for physical health. As a result, insurers are pushing for greater documented effectiveness of treatment.
Are Some Practices More Evidence-Based than Others?
Semantically, a practice can be deemed ‘evidence-based’ if there is almost any type of study or research to support it. As we indicated in a previous post, all evidence is not created equal. There is a wide spectrum of evidence types ranging from ‘Promising’ anecdotal and observational data to “Well-Supported” and rigorous systematic reviews and meta analyses.
The Substance Abuse and Mental Health Services Administration (SAMHSA) operated a database of research evidence on mental and behavioral health treatments. Known as The National Registry of Evidence-Based Programs and Practices (NREPP), the project ran for 20 years before being defunded in 2017. At the time of its shuttering, the NREPP included several hundred practices and programs for the treatment of substance use disorder.
The Pew Charitable Trust operates the Results First Clearinghouse Database, “an online resource that brings together information on the effectiveness of social policy programs from nine national clearinghouses.” Results First is far more broad than just Substance Use Disorder and Mental Health, but it does include most of the underlying research that was previously available through the NREPP.
However, at this time there is no single authoritative body that defines which among these hundreds of practices are “best” or most well-supported by research evidence. As such, the answer to this article’s title question is not black and white. Despite this, there are some practices which routinely appear on nearly all lists of evidence-based practices for substance use disorder. We are using a list of eight behavioral therapies from the advocacy group Shatterproof, who are spearheading an ambitious endeavor to certify treatment programs based on their usage of evidence-based practices, among other criteria. Shatterproof’s ATLAS project aims to be much more than just a database of treatment providers. It seeks to assess treatment facilities based on a set of objective criteria and to “provide transparent information on whether facilities offer services that align with evidence-based best practices that are shown to improve patient outcomes.” The project is funded by a coalition of various stakeholders including non-profit foundations and insurance companies. In designing the criteria for ATLAS, Shatterproof references practices listed by the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism.
The therapies listed in the Treatment Facility Survey are drawn from the National Institute on Drug Abuse (NIDA) and National Institute on Alcohol Abuse and Alcoholism (NIAAA) lists of evidence-based behavioral therapies, and are the only interventions that currently meet the following level of rigor as of October 2019: efficacy demonstrated in treating an SUD from at least 2 independent randomized controlled trials and a large-scale real world field trial.
We’ve labeled these treatments as ‘consensus’ to indicate the wide approval and endorsements they have received.
What Are the ‘Consensus’ Evidence-Based Practices?
Cognitive Behavioral Therapy (CBT):
CBT is both a standalone therapy as well as a technique used to engage individuals with other evidence-based practices. In their primer on CBT, SAMHSA describes it as:
[A] general classification of psycho-therapy, based on social learning theory, which emphasizes how our thinking interacts with how we feel and what we do. It’s based on the view that when a person experiences depression, anxiety, or anger that these stressors can be exacerbated (or maintained) by exaggerated or biased ways of thinking and that these patterns can be modified by reducing erroneous and maladaptive beliefs. A counselor using CBT helps a client to recognize their style of thinking and to modify it through the use of evidence and logic.
In lay terms, CBT attempts to mitigate problematic behavior (such as substance use disorder) by investigating the thoughts, feelings, and beliefs underlying that behavior. CBT strives to address the behavior by teaching coping strategies that address the emotional and behavioral cues that drive the substance use. There are two main components to CBT:
Functional Analysis/Self-Observation: Analysis of high-risk situations to provide insights into what may trigger or drive an individual’s substance use. Often, this starts with the counselor and client delving into a recent episode of substance use. The goal is for individuals to cultivate the skills of self-monitoring and self-evaluation to see the risky situation and what is driving it.
Skills Training: Having identified risky situations, CBT strives to replace old habits associated with substance use with healthier coping strategies and skills. In addition to addressing urges to use or drink, CBT skills can improve interpersonal relationships and help individuals learn to better tolerate feelings like fear, anxiety, anger, and depression.
Contingency Management:
Contingency Management seeks to reinforce positive behaviors through tangible rewards. There are two main types of contingency management.
Voucher Based Reinforcement (VBR) uses vouchers or gift cards for each drug-free urine sample provided. Voucher values increase with each consecutive clean urine test and reset in the case of a positive result.
Prize Incentives Contingency Management operates in a similar manner but offers a chance to win cash and prizes for negative drug screens, treatment attendance, or completing incremental treatment goals.
Studies have shown the practice is effective in supporting abstinence as well as treatment retention. A 2006 systematic review of 47 controlled studies of Contingency Management concluded the following:
“Study findings suggest that CM is among the more effective approaches to promoting abstinence during the treatment of substance use disorders. CM improves the ability of clients to remain abstinent, thereby allowing them to take fuller advantage of other clinical treatment components.” (Prendergrast et al., 2006)
Community Reinforcement Approach (CRA) plus Vouchers:
CRA combines several treatment components in seeking to make a non-using lifestyle more attractive than substance use. The core of CRA uses reinforcement in various spheres of an individual’s life to construct a ‘community’ around the person to support and reinforce the adoption of the new lifestyle. Components of CRA include the following:
Building motivation for change and helping to initiate abstinence.
Analyzing patterns of drinking, using, and other target behaviors.
Increasing positive reinforcement around healthy lifestyle choices.
Developing new and healthier coping skills and strategies.
Involving significant others (family, friends, employers, etc…) to construct a supportive community around the individual.
CRA is often combined with vouchers or prize incentives as in Contingency Management. CRA also leverages the core CBT techniques of Functional Analysis and Skills Training. In the case of CRA, the functional analysis helps identify both the behaviors intended to change as well as the most attractive incentives to use for reinforcement. Skills building is broad-based and includes hard skills such as vocational training.
Motivational Enhancement Therapy (MET):
MET seeks to build and strengthen an individual’s motivation to change and resolve any ambivalence toward treatment and substance use. MET is based on the principles of motivational psychology and employs techniques associated with Motivational Interviewing. As with the other treatment strategies on this page, MET is geared toward generating internally-motivated change. Instead of trying to teach a step-by-step method, MET seeks to show clients how to use their own internal resources in an adaptable way.
Research has shown that MET results in a sustained decrease of substance use and is particularly effective for alcohol use disorders (AUD). Studies have also shown that MET effectiveness can vary across different sites and populations.
The Matrix Model:
The Matrix Model was originally designed for engaging stimulant abusers in treatment and helping them to achieve abstinence. As the name implies, the matrix model utilizes multiple treatment strategies under one umbrella. These components include psychoeducation around addiction, family behavior therapy, relapse prevention strategies, individual counseling, and 12 step facilitation (TSF) therapy. As with many other treatments, the Matrix Model uses Cognitive Behavioral Therapy techniques to help motivate change, initiate action, and cultivate greater self-monitoring, self-evaluation, and self-regulation. Practitioners function as both teacher and coach to provide encouragement and positive reinforcement.
Although the original target population was stimulant users, it has since been applied effectively for treatment of other substance use disorders as well as the treatment of co-occurring disorders. Many treatment programs use a multi-component approach of education, counseling, relapse prevention, and fostering interaction with 12 step or other social support group. However, the Matrix Model is a specific and manualized intervention, meaning there is an explicit structure and specific components which are to be adhered to in order to maintain fidelity and to generate the type of results seen in the evidence base. Simply addressing the same components as found in the Matrix Model is not equivalent.
Family Behavior Therapy:
Family Behavior Therapy (FBT) is aimed toward addressing not only substance use disorder but also co-occurring problems. FBT combines behavioral therapies with contingency management techniques. Counselors engage families and significant others in applying the behavioral strategies. Patients are encouraged to develop behavioral goals that are anchored to a contingency management system. Rewards for achieving specified goals are provided by significant others. The goal is to acquire new skills both for treating substance use disorder and to improve the home environment.
Mindfulness-Based Relapse Prevention (MBRP):
MBRP combines skills-building approcahes from Cognitive Behavioral Therapy (CBT) with mindfulness practices. The goal is to develop a more flexible mindset to replace automatic responses to triggers, cues, or cravings. All relapse prevention strategies utilize some form of self-observation for identifying when one may be at risk of returning to active use. MBRP emphasizes the use of mindfulness practices to cultivate the awareness of oneself and one’s environment. Additionally, mindfulness practices promote a non-judgmental approach toward one’s feelings and actions and seek to make individuals more accepting of discomfort. By doing so, MBRP replaces automatic responses with a pause so one can analyze a situation in a mindful manner and ease the path to plan and take corrective action. Mindfulness acts an effective emotion regulation technique and so helps reduce the intensity of emotional triggers as well as providing a technique for addressing such triggers.
Twelve-Step Facilitation (TSF) Therapy:
The NIDA defines TSF as, “an active engagement strategy designed to increase the likelihood of a substance abuser becoming affiliated with and actively involved in 12-step self-help groups, thereby promoting abstinence.”
Please take a look at our previous Evidence-Based Blog article, “What Did That Big Alcoholics Anonymous Study Really Study?” for more detailed discussion of the intervention and recent research on the effectiveness of TSF.
Questions to Explore - Upcoming Articles on EBP
Thinking about your own practice or organization….
How broadly are you using evidence-based practices?
Which specific evidence-based practices are you currently using?
What barriers or obstacles have you encountered in implementing evidence-based practices?
Do you or your organization have a criteria for selecting evidence-based practices?
Future articles in the Evidence-Based Blog Series will include:
Implementation - How do I successfully go from identifying a practice supported by robust evidence to putting that practice into action in a real world setting?
Motivational Interviewing - Motivational Interviewing is a technique for cultivating motivation in individuals and eliciting a commitment to change. Many evidence-based practices provide a structure and Motivational Interviewing techniques inform the application of that framework.
Medication-Assisted Treatment (MAT) - There is a great deal of rigorous research supporting the power of medication to engage and retain individuals in treatment. Is MAT itself a ‘treatment’ or does it simply lay the groundwork for other treatments?
References
Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101(11):1546‐1560. doi:10.1111/j.1360-0443.2006.01581.x
Nowinski, J., Baker, S., & Carroll, K. M. (1992). Twelve step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence (Vol. 1). Diane Publishing Company.
NIDA. (2018, January 17). Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition). Retrieved from https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition
Substance Abuse Mental Health Services Administration & Office of the U.S. Surgeon General (2016). Facing addiction in America: the Surgeon General's report on alcohol, drugs, and health.
Author: Geoff Wilson. Use of this article for any purpose is prohibited without permission by Geoff Wilson.
Images Copyright 2023 R1 Publishing LLC / All Rights Reserved.
Here are a few ideas to help you learn more about R1 and engage others on this topic:
Share this blog post with others. (Thank you!)
Start a conversation with your team. Bring this information to your next team meeting or share it with your supervisor. Change starts in conversations. Good luck! Let us know how it goes.
Visit www.R1LEARNING.com to learn more about R1, the Discovery Cards, and how we’re creating engaging learning experiences through self-discovery.